Download case study
Project lead: Dr Kim Kavanagh, University of Strathclyde
Scottish researchers looked at how likely it is to develop a Clostridium difficile infection after having taken one or several courses of antibiotics in the past.
The Challenge
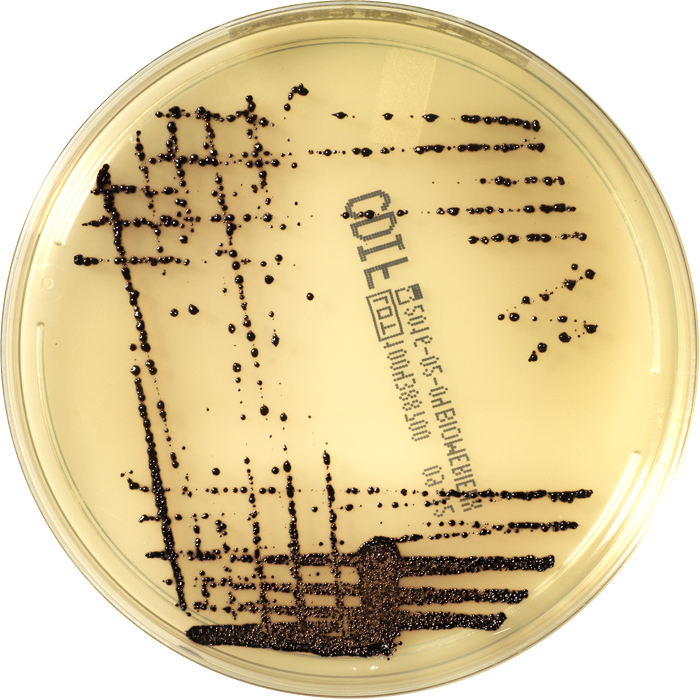
Clostridium difficile (C. difficile) is a bacterium that naturally occurs in the human gut. It can exist in the gut without causing any symptoms but it can also produce symptoms which can be life threatening.
C. difficile infections often arise when a patient is given a course of antibiotics which destroy many of the other ‘good’ bacteria living in our guts, thus removing competition for C. difficile which then starts to multiply.
The bacterium is resistant to a lot of antibiotics and can form spores which can’t be destroyed by antibiotics. These spores are tough and can remain in the environment for a long time. It’s therefore important to find out just how long patients are still at risk of getting an infection after receiving antibiotics.
The Research
A team made up of researchers from several Scottish universities looked at all C. difficile cases in Scotland recorded between 2010 and 2013, then narrowed these down to those 1,446 patients who had contracted the infection outside of hospital.
Identifying these cases was made easier by the Infection Intelligence Platform (IIP), which combines data from several different NHS databases.
Next, the researchers looked at the patients’ health records to see if and when they had been treated with antibiotics.
The Results
The researchers found that around 60 percent of patients with a C.difficile infection had taken antibiotics in the past six months, which is similar to the results of previous studies. One of their new findings however was that patients were at risk of getting a C. difficile infection even 4-6 months after they were last given antibiotics.
The Impact
The paper shows that repeated exposure is important as a risk factor for developing C. difficile infection. This result is significant because it means that it’s not just when antibiotics are prescribed long term (e.g. as a preventative measure when a person’s spleen has been removed) that increase your risk, but also if you have several short-term treatments with antibiotics.
This study once again shows the risks associated with antibiotic use and should encourage clinicians to think carefully about the risk versus benefits of prescribing antibiotics.
Kavanagh, K, Pan, J, Marwick, C, Davey, P, Wiuff, C, Bryson, S, Robertson, C & Bennie, M 2016, ‘Cumulative and temporal associations between antimicrobial prescribing and community-associated Clostridium difficile infection: population-based case control study using administrative data‘ Journal of Antimicrobial Chemotherapy. DOI: 10.1093/jac/dkw528
For more information about C. difficile infections visit:
www.nhs.uk/conditions/Clostridium-difficile
Enquiries to Sabine Kurz, Communications Assistant, The Farr Institute of Health Informatics Research, sabine.kurz@ed.ac.uk